<< Back
‘Flattening the COVID-19 Curve’: When Will it Happen?
March 25, 2020
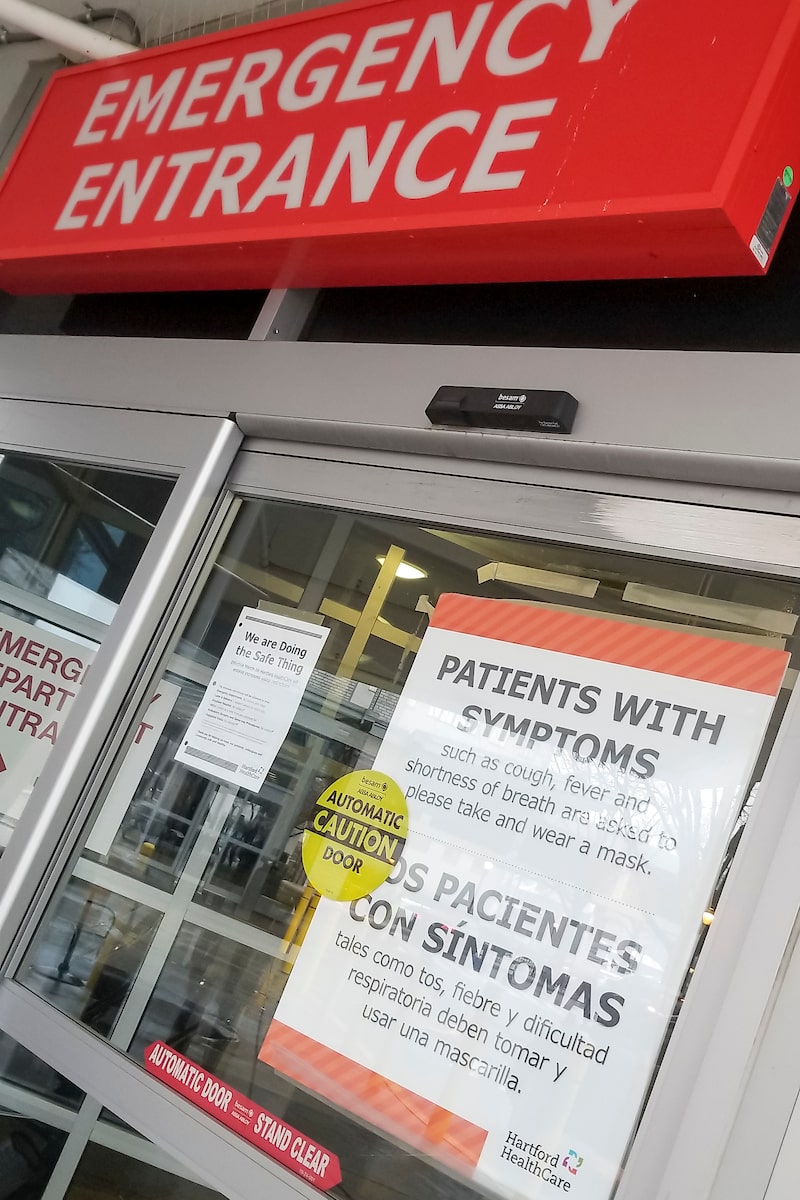
Dr. Ajay Kumar, Chief Clinical Officer with Hartford HealthCare (HHC), offered this update March 25 on COVID-19 testing, personal protection equipment (PPE) donations and surge planning on Wednesday. He then fielded questions from local media.
Using the word “optimistic” more than once regarding the COVID-19 pandemic, Dr. Kumar said thoughtful planning has positioned Hartford HealthCare to give every colleague working in clinical areas a protective mask to wear.
While strained supplies make the choice difficult, he said protecting front-line staff is paramount.
“Our job is to protect our colleagues who are there to provide care,” he said, noting the directive applies to all staff. “Whether they’re serving a meal or restocking supplies in the pharmacy clinical areas, they will get a mask.”
Monitoring personal protective equipment supplies is ongoing as the system sees increased numbers of COVID-19 patients and prepares to scale up capacity further for the anticipated surge, he said.
Dr. Kumar also said the system has expanded virtual health capabilities at its primary care practices and started screening all employees reporting for work at St. Vincent’s Medical Center for signs of COVID-19 infection. That practice will be expanded across the system “to protect our patients and colleagues.”
“This thoughtful, sequential approach positions us differently than other places across the country,” he said.
Q: How long can the masks last?
A: If staff is managing a COVID patient, it’s a single use. Otherwise, it can last several times and be reused, maybe even for a whole shift. It’s a complex operation. The N95, if cleaned and providing the right setting, can be reused.
Q: What other equipment is running out?
A: I wouldn’t say running out, I’d say we have a shortage of gloves, gowns, face shields. Gloves are a challenge because they’re made in China. We have enough for some time but those are the areas we worry about.
Q: How many masks do you need?
A: The numbers are arbitrary but I’d say 12,000 to 15,000 masks per day.
Q: What about home-made masks?
A: We have to be very cautious. In a healthcare setting, there are certain requirements. I would not permit these at this time.
Q: I’ve talked to nurses who are saying there are not enough PPEs.
A: I meet with my nursing colleagues all the time and it’s not what I’m hearing at this time.
Q: What percentage of your COVID-19 patients are in the ICU?
A: About 20 to 30 percent are in the ICU.
Q: How are they being treated if they’re not in the ICU?
A: They’re getting oxygen therapy, nebulizer treatments, Tylenol for the fever. We’ve also had several patients who have recovered and went home.
Q: What do you say to people about protection concerns for frontline staff?
A: We have had no staff exposed and test positive because of exposure to a patient. All of our policies and strategies so far have been working. We revised the screening criteria so when people show up, they are triaged in a closed setting so all the staff are aware of the risk. We’re also adding gastrointestinal signs to screening. Anyone assumed to be COVID positive is managed in a separate track to prevent exposure, preserve PPEs and get the patient the right care.
Q: How many staff have been tested and are positive?
A: About 60 have been tested. Some have been positive but all through community acquisition.
Q: What do you think the next two weeks will hold?
A: My best assessment is that we’ll have an increase in the numbers in the next two to three weeks in all healthcare facilities in Connecticut and an increase in hospitalizations. But, however, if we stick to social distancing, which we are doing very well, if we stick to our hand hygiene, if we stick to all the measures that are talked about in healthcare facilities and outside, I think there’s a very good chance that in about three to four weeks down the line we might see more flattening of the curve and a manageable situation happening.
I’m actually optimistic at this time that with all the things we have done, all the measures we have taken, despite us seeing some increased activity, we might a flattening curve provided we stay with things we’re doing at this moment and we continue to tighten our processes.
Q: Who is getting tested?
A: There are two groups – inpatients and colleagues suspected of being infected; and outpatients who are found to be most vulnerable to the disease. People do not have to be tested if they have cold-like symptoms. They can self-isolate.
Q: How can you reuse N95s?
A: In situations where you’re a nurse in a critical care space but not with COVID-19 patients, and the N-95 is not soiled, wet or fraying, it can be reused.
Q: Is 10 people in gatherings too many?
A: The 6-foot distance (between people) is more important. Social distancing is what’s going to manage this.
Q: Could staff members be COVID positive but have no symptoms?
A: It’s always possible, but that’s why we put significant barriers in place and take precautions with PPEs.
Not feeling well? Call your healthcare provider for guidance and try to avoid going directly to an emergency department or urgent care center, as this could increase the chances of the disease spreading.
Click here to schedule a virtual visit with a Hartford HealthCare-GoHealth Urgent care doctor.Stay with Hartford HealthCare for everything you need to know about the coronavirus threat. Click here for information updated daily.
Questions? Call our 24-hour hotline (860.972.8100 or, toll-free, 833.621.0600).
Get text alerts by texting 31996 with COVID19 in the message field.